CDC: “Superbug” Speads To 35 States; Kills Upwards Of 40% Of The People Who Come In Contact

This is possibly our biggest infection control dilemma yet. Although cases of this bacterial infection has been on the rise worldwide for the last 10 years, there is an alarming spread recently across the US. Thirty-five states have reported the outbreak, but there could be more in states not required to report it. What makes this opportunistic “superbug” such a nightmare is that it is Carbapenem-Resistant, meaning “last resort antibiotic” resistant. It’s a Carbapenem-Resistant Klebsiella pneumoniae (CRKP); Klebsiella pneumoniae is a strain of Klebsiella which is related to E. Coli and Salmonella from the family Enterobacteriaceae.
Found inside the gut, outside of the gut, it can cause lethal infection. The major reservoirs of infection are the gastrointestinal tract of patients, catheters, unclean instruments, and the hands of hospital personnel. It zeros in on hospitals, ICUs, long term care faciities like nursing homes, and those with immuno-compromised conditions. It is a potential community-acquired type of pneumonia (different, not acquired from hospitals) and the bug has an incredible ability to mutate and resist. It does indeed carry a fatality rate between 35 and 50 percent or more.
Are we just to avoid hospitals and nursing homes to keep from this public threat? While CRKP and other resistant strains laugh in the face of antibiotics, there is some glimmer of hope. As of 2005, the EPA registered chlorine dioxide (aka MMS) as a disinfectant for MRSA. Pathogens cannot resist it and it does not harm humans. Unlike bleach, it requires very small concentrations, and leaves no residue. It completely breaks down thick cell walls which is one of the reasons these superbugs are so resistant.
As of 2006, Purdue University researchers found that besides laser detection technology,
“A second innovation uses chlorine dioxide gas to kill pathogens on produce, fresh fruits and vegetables. This would be a large step up from current technologies, which mainly involve washing and scrubbing, and cannot completely rid a product of a pathogen like E. coli,” said Richard Linton, a professor of food science.
“We can use the laser technology to detect problems more quickly, determine exactly what the pathogen is and where it came from,” Linton said. “As for using this gas as a disinfectant, I would say that in my 13 years of doing research, it is 10,000 to 100,000 times more effective than any process I have seen.”
It is not clear at this time if hospitals are rigorously trying to control the bug with this disinfectant. Let’s hope that hospitals, nursing homes and others not forget this lifesaving preventative and controller.
~Health Freedoms
The CDC and LA Times reports a “Superbug” that kills 40% of the people it comes in contact with has hit 35 US States and is now being spread through California medical facilities.
LA Times:
A dangerous drug-resistant bacterium has spread to patients in Southern California, according to a study by Los Angeles County public health officials.
More than 350 cases of the Carbapenem-Resistant Klebsiella pneumoniae, or CRKP, have been reported at healthcare facilities in Los Angeles County, mostly among elderly patients at skilled-nursing and long-term care facilities, according to a study by Dr. Dawn Terashita, an epidemiologist with the Los Angeles County Department of Public Health.
It was not clear from the study how many of the infections proved fatal, but other studies in the U.S. and Israel have shown that about 40% of patients with the infection die. Tereshita was not available for comment Thursday morning but was scheduled to speak about the study in the afternoon.
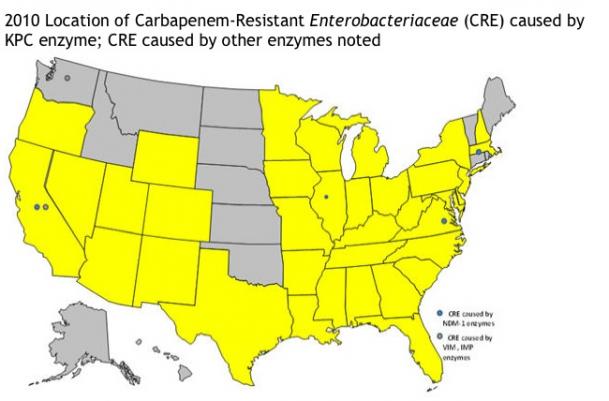
Here’s a map from the CDC of states where it has been reported:
The Centers for Disease Control Writes:
Public Health update of Carbapenem-Resistant Enterobacteriaceae (CRE) producing metallo-beta-lactamases (NDM, VIM, IMP) in the U.S. reported to CDC
Given the importance of Enterobacteriaceae in healthcare-associated infections (HAI) and the extensive antimicrobial resistance found in these strains, all types of carbapenem-resistant Enterobacteriaceae (CRE) are an important public health problem, regardless of their mechanism of resistance or their country of origin. In addition, as Enterobacteriaceae are a normal part of human flora, the potential for community-associated CRE infections also exists. Carbapenem-resistance in Enterobacteriaceae can occur by many mechanisms, including the production of a metallo-beta-lactamase (such as NDM, VIM, and IMP) or a carbapenemase (such as Klebsiella pneumoniae carbapenemase, KPC).
CDC has been working with partners to prevent CRE infections, including those caused by KPC-producing organisms, which are the most common type of CRE in the United States. The KPC gene makesEnterobacteriaceae bacteria resistant to all beta-lactam/carbapenem antibiotics. KPC producers have been reported in about 35 states and are associated with high mortality, up to 40 percent in one report. They may be present in the other 15 states as well, but have not been reported to CDC. The presence of CRE, regardless of the enzyme that produced that resistance, reinforces the need for better antibiotic stewardship, transmission prevention, and overall HAI prevention in any healthcare setting.
The detection of new mechanisms of carbapenem resistance (ie, metallo-beta-lactamases) in the United States has raised questions about the identification and control of CRE. The mechanism of carbapenem-resistance is of epidemiologic interest but is not necessary for implementation of infection prevention recommendations. Current guidance for the control of all types of epidemiologically important multidrug-resistant organisms is available in the2006 MDRO Guideline. In addition, see specific guidance for the control of CRE. These recommendations apply regardless of the resistance mechanism.
It is important to note that CRE, unlike other drug-resistant infections such as VRSA, are not a nationally reportable or notifiable disease. Therefore, there is not a requirement to report to CDC and therefore we may not know the true number of infections caused by these organisms in the US (only those voluntarily reported to CDC).
States with confirmed CRE cases caused by the KPC enzyme.
Alabama
Arizona
Arkansas
California (CRE caused by the NDM-1 enzyme and VIM or IMP enzyme)
Colorado
Delaware
Florida
Georgia
Illinois (CRE caused by the NDM-1 enzyme)
Indiana
Iowa
Kentucky
Louisiana
Maryland
Massachusetts (CRE caused by the NDM-1 enzyme)
Michigan
Minnesota
MississippiMissouri
Nebraska
Nevada
New Hampshire
New Jersey
New Mexico
New York
North Carolina
Ohio
Oregon
Pennsylvania
South Carolina
Tennessee
Texas
Utah
Virginia (CRE caused by the NDM-1 enzyme)
West Virginia
Wisconsin
WyomingState(s) with confirmed CRE cases caused by a VIM or IMP enzyme
Washington
By Alex Higgins, The Intel Hub
http://www.infowarhorse.com/cdc-%E2%80%9Csuperbug%E2%80%9D-speads-to-35-states-kills-upwards-of-40of-the-people-who-come-in-contact/
Sources:
http://news.uns.purdue.edu/html4ever/2006/061005LintonFood.html
http://www.shareclean.com/news/new21.html
http://www.ourfood.com/General_Bacteriology.html#S051140000
http://www.medicalnewstoday.com/articles/30105.php
http://www.medicalnewstoday.com/articles/205672.php
http://www.cdc.gov/ncidod/eid/vol8no2/01-0025.htm
http://www.cdc.gov/ncidod/eid/vol8no2/01-0025.htm
http://latimesblogs.latimes.com/lanow/2011/03/superbug-spreading-to-southern-california-hospitals.html
http://www.cdc.gov/HAI/organisms/cre.html
Health Freedom Alliance
Health & Wellness Foundation
CHAD Foundation
http://www.healthfreedomalliance.org