Non-surgical procedure repairs severed nerves in minutes
By Brian Dodson
21:41 February 7, 2012
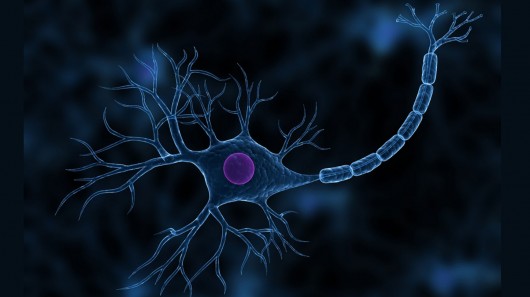
U.S. researchers have developed a nonsurgical technique to repair severed nerves in minutes instead of months (Image: Shutterstock)
Professor George Bittner and his colleagues at the University of Texas at Austin Center for Neuroscience have developed a simple and inexpensive procedure to quickly repair severed peripheral nerves.
The team took advantage of a mechanism similar to that which permits many invertebrates to regenerate and repair nerve damage. The new procedure, based on timely application of common chemicals to the severed nerve ends, could help patients to recover nearly full function in days or weeks.
Peripheral nerves connect the central nervous system to the muscles and sensory organs. Nerves contain a bundle of cylindrical sheaths called axons, within which reside individual nerve cells. The axons are surrounded by Schwann cells which coat the axons with myelin.
Trauma to peripheral nerves is relatively common. A nerve that has been damaged by pressure or stretching generally has a severed nerve fiber inside an intact axon. A severed nerve occurs when both the nerve fiber and the axon are cut in two. Either injury can prevent muscles from working and result in loss of feeling from the area of the body served by that nerve, often for years thereafter.
Why is nerve repair in mammals such a slow process?
When a nerve fiber breaks within its axon, the broken end of the nerve fiber which is no longer connected to the central nervous system dies, leaving an empty axonal tube from the point of injury. The nerve fiber will slowly grow within the empty tube, at a rate of about an inch per month. Thus, even minor nerve injuries commonly take months or years to heal. Even then the regrown nerves rarely meet up perfectly with the original muscles and sensory organs, so that a significant amount of function is permanently lost.
In what is known as Grade V neurotmesis, the axon is severed along with the nerve fiber. The growth of the regenerating nerve fiber is not constrained, and can form a twisted ball of nerve fiber at the cut in the axon. Such nerve scars are called neuroma, and can be extremely painful. Recovery from Grade V nerve injury is never rapid, usually taking months or years for even partial recovery.
In current medical practice, a cut nerve is repaired by using microsutures to reconnect the cut ends of the axon in an extraordinarily delicate operation (imagine sewing together two limp strands of angel hair pasta).
The object is to provide a continuous axon to guide the regrowth of the nerve fiber. Again, the regrowth process takes months or years to be completed, and typically the function of the original nerve will remain impaired.
A new approach
Professor Bittner's team had discovered earlier that when a plasma membrane is damaged, a calcium-mediated healing mechanism starts to draw small vesicles toward the site of the injury. Vesicles are small sacks made of lipid membranes which provide the material needed to repair an injured plasma membrane. However, when the vesicles are attracted to the site of a severed axon, both ends of the axon are sealed off by this repair mechanism, preventing regrowth of the nerve.
To avoid this problem, the first step of the Texas group's nerve repair procedure is to bathe the area of the severed nerve with a calcium-free saline solution. By removing calcium from the injured axons, premature healing of the axon ends by this vesicle-based repair mechanism is prevented and even reversed. The damaged axons remain open, and can more easily be reattached. The calcium-free solution also contains antioxidants (e.g., methylene blue) to prevent degenerative changes in the axon and nerve.
In standard methods, the two ends of the severed axon would be reattached surgically. In contrast, Bittner's procedure does not require such difficult microsurgery. Instead, the severed ends of the axon are pulled to within a micron of each other, whereupon a small amount of a solution containing polyethylene glycol (PEG) is injected. The PEG removes water from the axonal membranes, allowing the plasma membranes to merge together, thereby healing the axon.
At the same time, the nerve fibers are brought into close enough proximity that they receive chemical messengers from each other making them believe they are still whole, thereby preventing the death of the disconnected nerve fiber. The severed nerve fibers can then grow together in a short period of time and with relatively good fidelity to the original connectivity of the nerve fibers.
The final step of the procedure is to inject the area with a calcium-rich saline solution, which restarts the vesicle-based repair mechanism, thereby repairing any residual damage to the axonal membrane. At this point, the nerve is structurally repaired, and use of the affected area begins to return within a few hours.
Indeed, tests of Bittner's procedure on rats have indicated an amazing level of success. The sciatic nerve of the rats was cleanly severed, resulting in paralysis of the affected limb.
Within minutes of awaking from Bittner's procedure, many of the rats were immediately able to move the limb containing the severed nerve. The normal function of the limb was partially restored within a few days, and 80-90% of the pre-injury function was restored within two to four weeks. Control rats subjected to sciatic nerve cutting followed by a sham procedure permanently lost nearly all (95-98%) function in the affected limb.
The chemicals used in Bittner's procedure are common and well understood in interaction with the human body. PEG is on the FDA's GRAS (generally recognized as safe) list, and methylene blue is an aromatic dye used for staining histological samples, as well as in fabric stains and paints. Because of this, there is no clear obstacle to beginning human clinical trials of the procedure. Indeed, teams at Harvard Medical School and Vanderbilt Medical School and Hospitals are currently conducting studies aimed at gaining approval for such trials. While the procedure developed by Bittner's group will not apply to the central nervous system or spinal cord injuries, the procedure offers hope to people whose futures include accidents involving damaged nerves.
Sources: University of Texas, News in Physiological Sciences
Copyright © gizmag 2003 - 2012 To subscribe or visit go to: http://www.gizmag.com