Brain cells created from human skin cells offer potential MS treatment
By Ben Coxworth
February 12, 2013
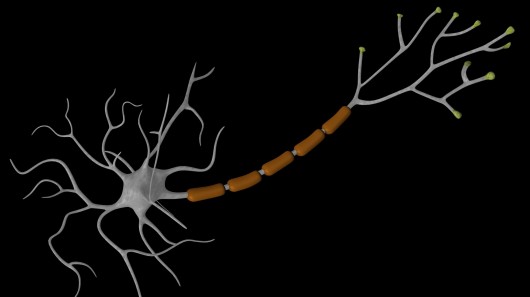
Myelin is a fatty tissue that covers the fibers between nerve cells – it’s not unlike the insulation on electrical wiring. When that tissue is compromised, the cells have difficulty communicating, and neurological diseases such as multiple sclerosis can be the result. If the myelin of MS sufferers could be regrown, then it’s possible that the disease could be cured. Recently, a team of scientists successfully regenerated myelin in mice, using human skin cells that were reprogrammed into brain cells.
Quite often when we hear about stem cells – the “blank slate” cells that can be turned into just about any type of bodily cell – they’re obtained from embryos or umbilical cord blood. Along with the logistic (and possibly ethical) challenges involved in obtaining the raw material, the resulting tissue cells may not be accepted by a recipient’s immune system.
It’s also possible, however, to convert – or perhaps more accurately revert – adult somatic cells into what are known as induced pluripotent stem cells. Because the patient’s own skin, stomach, liver, or blood cells can be used, there’s plenty of readily-available material at hand, and rejection is much less likely.
In the recent study, a team led by University of Rochester Medical Center neurologist Steven Goldman converted human skin cells into human induced pluripotent stem cells (hiPSCs), that were in turn made to become oligodendrocyte progenitor cells (OPCs). Myelin cells in the brain and spinal cord are produced by cells known as oligodendrocytes, which are themselves produced by OPCs. Therefore, it was hoped that by introducing the engineered cells into someone with MS, their myelin could be regrown.
It took four years to establish a reliable method of converting sufficient quantities of skin cells into OPCs. The scientists then proceeded to transplant them into lab mice that were genetically incapable of producing myelin. The introduced cells spread through the animals’ brains and started production of myelin, yet without causing any tumors – a possible side-effect of some stem cell therapies. The treated mice were found to live “significantly longer” than their untreated counterparts.
Clinical trials on humans are planned to begin in 2015. A paper on the research was recently published in the journal Cell Stem Cell.
Source: University of Rochester Medical Center
Copyright © gizmag 2003 - 2013 To subscribe or visit go to: http://www.gizmag.com