A study from researchers at the Gladstone Institutes in San
Francisco has examined the protein BRCA1, using a combination of
tests on laboratory mice and human brain tissue to determine that
the protein is central to learning and retaining memories. The work
highlights the importance of the protein in relation to the
cognitive decline associated with Alzheimer's disease, and could
help in the development of future treatments.
Alzheimer's is a degenerative condition affecting some 5.3 million people in the US alone. We've seen numerous recent breakthroughs in the study of the disease, including drugs that attack aspects of old age associated with the condition, and the identification of the mechanism that causes synapses in the brain to break down as it progresses.
The new research focuses on the protein BRCA1. In the past, BRCA1 has been studied in dividing cells, where it plays a core role in repairing a type of DNA damage, called a double-strand break, wherein both strands of the double helix are severed.
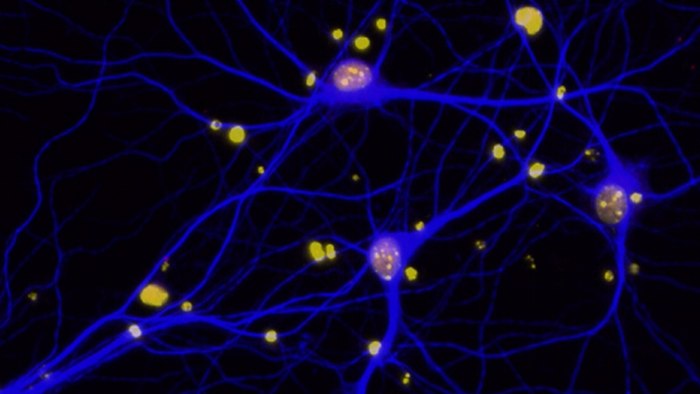
Things are a little different in the brain, with double-strand breaks occurring more regularly, and under normal conditions, such as following a period of increased brain activity. The Gladstone researchers theorized that the cycle of DNA damage and repair in the brain is actually what facilitates the learning process. Therefore, when decreased levels of BRCA1 are present, this function is disrupted, leading to impaired cognitive function – a hallmark of Alzheimer's disease.
To test this theory, the scientists reduced BRCA1 levels in neurons in laboratory mice. The results showed a build up of DNA damage, leading to a decrease in learning and memory. With the findings tallying up with the team's theory, it moved on to study the effect in specific relation to Alzheimer's disease.
To do so, the researchers analyzed neuronal BRCA1 levels in post-mortem Alzheimer's patient brains, comparing the findings with those taken from healthy tissue. They found that the levels of the protein were reduced by between 65 and 75 percent in the Alzheimer's patients' neurons – results that once again support the team's theory.
Having established that BRCA1 plays a big role in the degenerative condition, the researchers then approached the problem from a slightly different angle, recreating the process of the disease to determine what cause the depletion of the protein. They introduced amyloid-beta proteins, which are central to Alzheimer's disease, building up to form harmful plaques in the brain, to neurons grown in cell culture.
As expected, the amyloid-beta depleted the BRCA1 when introduced, strongly indicating that the protein, and its negative effects on BRCA1, are responsible for the faulty DNA repair witnessed in Alzheimer's patients' brains.
Lastly, the team used lab mice to demonstrate that increased amyloid-beta causes a decrease in BRCA1, but the next part of the study could well be the most exciting. Moving forward, the researchers will conduct tests on mice to see whether increasing BRCA1 levels can prevent, or even reverse, the cognitive deficit caused by the condition.
"Therapeutic manipulation of repair factors such as BRCA1 may ultimately be used to prevent neuronal damage and cognitive decline in patients with Alzheimer's disease or in people at risk for the disease," says study lead author Lennart Mucke. "By normalizing the levels or function of BRCA1, it may be possible to protect neurons from excessive DNA damage and prevent the many detrimental processes it can set in motion."
The findings of the study were published in the journal Nature.
Source: Gladstone Institutes